

No matter what kind of arthritis or related chronic illness you have, there’s no doubt that living with it is complex and complicated. Very often, our family and friends do try to understand what it’s like to live with our conditions, but the fact of the matter is that unless you have the disease, you can’t really grasp the full magnitude of it and the everyday challenges it brings.
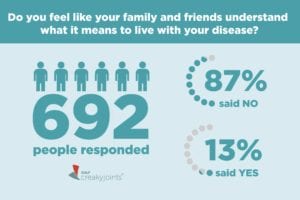
We wanted to understand how our community felt about this issue, so we asked ArthritisPower members in a recent Community Poll: Do you feel like your family and friends understand what it means to live with your disease?
Nearly nine in 10 of 692 respondents said they don’t.
Why Is Arthritis or Related Diseases So Hard to Understand?
“The complexity of disability is that it’s lived in the body, but it’s also experienced throughout everything else in life,” says Linda Mona, PhD, a licensed clinical psychologist with Inclusivity Clinical Consulting Services, whose research focuses on the diverse life experiences of individuals living with chronic health conditions/disability. “Family members might see that it takes somebody two hours to get ready in the morning, but I don’t know that they understand what it’s like to live their day in society. From the minute you leave the door to the minute that you come home, there are barriers and obstacles in the environment and in other people’s attitudes that pummel you throughout the day.”
There are many possible reasons why arthritis is so hard for those without it to truly understand, but common issues have to do with misperception related to disease severity, invisibility, unpredictability, and how we as a culture think about pain.
Misperception of disease severity
“The whole area of arthritis is so widely misunderstood,” says clinical psychologist Laurie Ferguson, PhD, director of education development for CreakyJoints. “It is considered your grandparent’s disease — you’re just a little stiff, or you just have aches and pains. It requires constant education to help people who don’t have arthritis understand the gravity of it.”
The gravity can relate to many different aspects of living with a chronic illness: severe pain, fatigue, comorbid conditions such as heart disease, medication access challenges, the inability to work or be as independent as you’d like, to name just a few.
Invisibility
Some people with arthritis show visual clues that may help convey that they’re in pain: They may use a cane or a wheelchair, their gait may be affected, or they may have structural damage in their hands or other areas. But many people with arthritis look “normal” on the outside. “This puts a huge responsibility on people with non-apparent disabilities for disclosure,” says Dr. Mona, who herself has lived with chronic health issues since the age of 6 and has used a scooter wheelchair since age 14.
“Someone has to tell you they’re in pain, or there’s fatigue, or they don’t think they’re going to be able to [participate in something],” says Dr. Ferguson. “Nobody’s just going to notice it by looking at you.”
Unpredictability
Arthritis symptoms come and go. A person can wake up feeling fine and be in the midst of a flare hours later. This changeability can be hard for others to comprehend. “[Arthritis] is unpredictable for patients, so it’s also unpredictable for their families and their friends,” says Dr. Ferguson.
Perception of Pain
The word “pain” is a loaded one, because everyone has had their own experience with pain, which in turn affects how they feel about the pain that others experience. “People’s interpretation of other people’s pain is often based on their own history or their own mythology of what pain is and how people should be able to stand it or bear it,” says Dr. Ferguson. “We live in a culture that is not empathetic to chronic pain, period.”
How to Feel Supported and Understood About Living with Arthritis
Even though it is challenging to feel like those around you truly understand what you’re coping with, there are things you can do to help increase others’ understanding of your experience with arthritis, as well as to better cope with moments when you don’t feel supported or understood. Consider this advice from Dr. Ferguson and Dr. Mona:
1. Start with self-compassion
This, Dr. Mona, says, is the most important step. “It is very hard to take a step back and have some self-compassion that life really is that hard sometimes,” she says. “There has to be space to feel upset and angry and that can sit next to all the other joys and hopes that people have. I think that having self-compassion is really important.”
Whether you’ve lived with arthritis for years or decades or have been diagnosed more recently, take a step back and recognize that you’ve been dealt a tough situation. Recognize that you’re entitled to feel a range of emotions about it. Recognize that not everyone will understand all the emotions you feel about managing a chronic disease, but they may try in their own way — and that’s OK.
2. Explore why you feel misunderstood
With a disease like arthritis, there’s a lot for others to unpack. People might not understand what fatigue really feels like or the guilt you feel about cancelling plans when you don’t feel up to something or the annoyance of not being able to do daily tasks like laundry. It may be difficult for others to understand the frustration you feel from not being able to exercise or play sports like you used to, or the anxiety you may have about whether your treatments are working or will continue to work in the future.
Reflect on what specifically it is that you feel misunderstood about, says Dr. Mona. “Then think about, what could I tell this person that might make a difference? What is it that I want this family member to know that they don’t know?” The next step is practicing ahead of time, or even preparing a mini mental script of how you can explain something.
“Plan ahead and say, ‘Okay, so I’m going to this family gathering, or I’m going to this friendship gathering and what can I anticipate that they’re going to ask me or that I might want to say?’” she suggests.
3. ID your ‘people’
Of course, constantly explaining yourself to others is exhausting. That’s why “it is essential that anyone living with arthritis have at least one person, preferably a couple of people, who ‘get it,’ so that they’re not spending a lot of time and energy trying to interpret how they feel,” says Dr. Ferguson. This could be a partner, best friend, or work colleague — but it also might NOT.
“You have to be realistic about finding the people who can get you. Maybe you wish your best friend, or your spouse, or your mother really got you, and that’s just never going to happen,” says Dr. Ferguson. This person could be a professional, such as a counselor or a religious leader.
The key is to look for someone who has what Dr. Ferguson calls “dispassionate empathy.” This means someone who can listen to you without necessarily trying to “fix” everything that’s wrong.
“Oftentimes, with people who love us, when we start to share with them that something’s painful or difficult, they can’t stand it and they immediately start trying to figure out what to do to make it better,” she explains. “Usually, that’s not the most helpful first response. Dispassionate means that I can hold your experience and care about you. I don’t have to make it better. I can listen and hold it, and you know that I’m witnessing it and I care.”
4. Create your own community
If you’re reading this and feel like you don’t necessarily have people in your life who offer you that dispassionate empathy you need, you can find those who can in the arthritis and chronic illness community. CreakyJoints Facebook, Twitter, and Instagram pages are good places to start. You can look for others that are specific to your disease as well.
“One of the things that helps safeguard those of us who live with disability and chronic health issues is being around community,” says Dr. Mona. “It is an emotional safety net for us. There’s something about feeling known by somebody else, by that shared experience, that is healing. To know that maybe sometimes our goal is not going to be trying to convince non-disabled people what they should know about us or why they should accept us, but it’s knowing that we are different and that difference is okay and that we can feel understood in some circles and that there are going to be other circles that are more of a challenge or where we’ll never be understood.”
5. Tell people how they can support you
No one is a mind reader. Even people in your life who understand and empathize with what you’re dealing with can benefit from direction and guidance from you about what you need.
“You might say to a loved one, ‘When I’m in pain I don’t need you to do anything for me necessarily. I just really want to be able to say it out loud,’” suggests Dr. Mona. “Or tell someone that you want to be able to say, ‘This is a bad disability day or a bad chronic health day. So, I’m really sorry I can’t commit to what I originally told you, but I just need you to understand that it’s real for me and I’m gonna have to pass on this.’”
6. Write about it
When it’s hard to express how you feel to other people, research shows that finding an outlet to write about it can be very helpful. You can blog online or post your thoughts on a social network, but writing in a private journal gives you the most freedom to be expressive. “Witness yourself, write down everything. Don’t hold back, don’t edit yourself,” says Dr. Ferguson. “Writing how you feel can be very helpful.”
7. Share articles that speak to you
If you’re not the writing kind — or not the kind to write publicly — another way to let people know how you feel or what you’re going through is to share relevant articles or essays on social media or via email.
“Let’s say you read an essay and think, ‘Oh my gosh, this is me,’ you can forward that to a couple of people and write, ‘I really resonated with this, and I thought maybe this might help you understand what I’m coping with,’” says Dr. Ferguson.
Both Dr. Ferguson and Dr. Mona acknowledge that it can be a burden to feel as though you have to constantly educate those around you about arthritis. Sharing content on social media could be a less invasive way of getting your point across.
8. Allow people to mess up
People may not always know the right thing to say. Even people with good intentions might say the wrong thing or be insensitive to your needs on occasion. “We have to be in a place where we allow people to make mistakes, or if they say something offensive, we have to give people the opportunity to repair,” says Dr. Mona. But the context and relationship matter. “Is the relationship important to you? Is it your mother? Is it your cousin? You might give somebody close to you a little bit more leeway that you would a random stranger off the street.”
9. Don’t give up
There’s something to be said for having a “this too shall pass” mentality when possible. You might be going through a tough time right now and feel particularly misunderstood or unsupported by those around you. Having hope and optimism that things will get better is key.
“Many people I work with in the arthritis community have that inner strength not to give up,” says Dr. Ferguson. “They both accept what’s going on with them and they keep trying to make it work the best they can for them. They’re willing to change doctors. They’re willing to really consider what medicines would be helpful to them. They work on relationships. They have hobbies. They do what they can to have a life that is not defined by their arthritis.”
Look for connections, relationships, and activities that bring you joy and belonging. “What psychology knows is that when we participate in pleasurable activities and have a sense of belonging, our well-being skyrockets,” says Dr. Mona. “And we need our well-being to skyrocket because we face a lot of obstacles in life. You want to try and enhance that as much as possible.”
Get Involved in Arthritis Research
If you are diagnosed with arthritis or another musculoskeletal condition, we encourage you to participate along with other patients like you in research studies by joining CreakyJoints’ patient research registry, ArthritisPower. ArthritisPower is the first-ever patient-led, patient-centered research registry for joint, bone, and inflammatory skin conditions. Learn more and sign up here.





